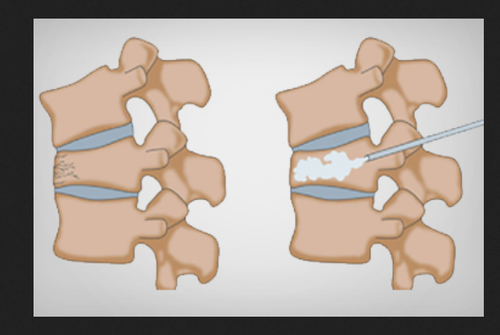
Vertebroplasty may be used for patients with vertebral compression fractures due to osteoporosis, metastatic tumors, or benign tumors such as vertebral heamangiomas. Patients with metastasis and myeloma usually experience severe pain and disability.
Vertebroplasty is performed to provide pain relief and to produce bone strengthening and vertebral stabilization when the lesion threatens the stability of the spine. Radiation therapy may be performed in conjunction with vertebroplasty. When the latter is performed for tumor lesions bone cement injection does not prevent tumor growths. Also radiation therapy does not interfere with the mechanical properties of bone cement and complements.
Vertebral hemangiomas are common benign lesions of the spine that are often asymptomatic and discovered incidentally during radiologic evaluation. Rarely, they may be painful, and there must be a close correlation between clinical findings and radiologic features to ensure that the patient’s pain is due to the vertebral hemangioma. In such cases, vertebroplasty is performed to provide pain relief. The PMMA is injected for pain relief, bone strengthening, and direct embolization of the hemangiomatous body.
Vertebral fractures are the most common complication of osteoporosis. Age-related osteoporotic compression fractures occur in more than 500,000 patients per year in the United States. About 15% of women in the United States older than 50 years of age will suffer one or more vertebra compression fractures related to osteoporosis. Patients most likely to benefit from vertebroplasty are those with a focal, intense, deep pain associated with evidence of a new or progressive compression fracture. Patients who seem to respond the best include those with a single level or a few levels for treatment, fractures that are present less than 2 months or a recent worsening of the fracture, and no significant sclerosis of the fractured vertebra. It should also be determined if the patient is able to tolerate lying prone for 1 to 2 hours.
Contraindications of vertebroplasty;
- Epidural involvement of the infiltrative lesion
- Coagulation disorders
- Extensive vertebral destruction
- Significant vertebral collapse with less than 1/3 of original height
- Radiculopathy into the lower extremity
- Disruption of the posterior vertebral wall
- Lesions above T 4
- Patients who cannot lie prone for prolonged period
Investigations:
Computed tomographic (CT) imaging for the diameter of the pedicles to be entered is helpful. Recent plain radiographs should be examined. Recent MRI should be available, particularly a T2-weighted sagittal image and axial views through the levels of pathology to be treated. In patients with multiple compression fractures, those vertebral bodies with enhancement demonstrate edema at that level and a greater likelihood of response.
Prothrombin time, partial thromboplastin time & platelet function studies.
Procedure:
The procedure is done under conscious sedation. Sedative analgesics like fentanyl, midazolam, or propofol are administered. Prior to the start of the procedure, a prophylactic antibiotic should be given intravenously.
The patient is taken to the fluoroscopy suite and placed in the prone position on the operating room table with all pressure points padded and standard monitoring applied. Care is taken to add extra padding to the table due to the osteoporotic spine and risk of rib fractures.
The level for the procedure is located in the posteroanterior fluoroscopic view. The fluoroscope is then rotated to an oblique position to maximize the oval appearance of the pedicle. Proper view is identified by seeing a “Scottie dog” appearance of the pedicle. It is important to “flatten out” the end plates of the vertebral bodies; if necessary, cephalocaudad or caudocephalad fluoroscopic angle may improve the image. This will locate the pedicle well within the vertebral body in the fluoroscopic view. It is important to oblique the fluoroscopic view enough to place the facet joint in the middle of the vertebral body and the spinous processes to the contralateral side. This facilitates a central placement of the needle. The target for entry is the superior lateral quadrant of the pedicle in the fluoroscopic view.
After the site of entry is identified, a skin is anaesthetized. A small skin incision is made with a No. 11 blade scalpel to allow insertion of a large bore biopsy needle. An 11 gauge bone biopsy needle is inserted through the incision. It is advanced in “gun-barrel” fashion in the oblique fluoroscopic view to monitor direction. The oblique view will show the needle shaft end-on as a circle within the center of the pedicle. Once contact has been made with bone, insertion through the cortex of the bone may be accomplished with a twisting motion of the needle or gentle tapping of the needle with a sterile hammer. It is important to “set” the needlepoint at the exact site of entry.
In the lateral view, the needle needs to be at the upper midpoint of the pedicle so that the needle advances in the midpoint of the pedicle. The needle should follow a path that is parallel to the superior and inferior edges of the pedicle. The needle is advanced to the junction of the anterior and middle third of the vertebral body. After placement of the needle, the cement is prepared for injection. The amount to be mixed is based on the clinical observation of an average of 7 to 8 mL of cement injected in a lumbar vertebral body. The liquid monomer is titrated until it takes on toothpaste like consistency. There are several delivery systems available that may be used to simplify the mixing and delivery in addition to decreasing fumes. If these systems are not available, I-mL syringes may be filled and used one at a time to inject the cement into the vertebral body. The injection of the cement is followed under fluoroscopic guidance in the lateral view. When the spread of the cement starts to invade the posterior one third of the vertebral body, injection should be stopped. The cement is 90% fixed at 1 hour.
After the procedure, the patient should be monitored for 3 hours in a recovery area prior to dismissal. The patient should be supine for 2 hours and then may sit. A CT image through the levels (2-mm slices) is recom�mended for documentation purposes. The patient is dismissed with routine pain medications and a graduated resumption of activity. Discharge instruction for the patient should include advice to call the physician for the following symptoms: New onset of back pain, Chest pain, Lower extremity weakness, Fever > 100F.
Complications:
Because of the size of the biopsy needle, there is risk of fracture of the lamina or pedicle. Preprocedural CT with pedicular diameter is helpful in assessing this risk. Owing to the vascularity of the vertebral body, there is the potential risk of pulmonary venous migration of the cement resulting in embolic phenomenon.
It is important to observe the spread of the cement under direct fluoroscopy to monitor for foraminal and/ or epidural extravasation. If vertebral epidural space extravasation occurs, there may be partial or com�plete paraplegia. Emergent operative decompression must be performed if the patient is symptomatic to min�imize any damage. This risk is more common with ver�tebral destruction of the vertebral body from malignancy.
An intradiscal leak of the PMMA may occur associ�ated with cortical fracture or osteolysis of the vertebral end plates. This does not seem to prevent pain relief. Secondary degenerative changes may develop because of this leak, but may not be deemed important due to the short life expectancy in these patients.
The PMMA may leak into the adjacent paraverte�bral tissue because of the cortical osteolysis of the verte�bral body or the hole produced by the needle after its removal. This may lead to a transitory femoral neuropathy due to a leak into the psoas muscle.
Aside from extravasation, the patient may complain of transient dermatomal pain due to rib fracture or mild nerve root compression. Osteoporotic patients may fracture a rib with a vigorous cough. It is imperative to carefully pad the operating room table to minimize this complication.
Conclusion:
Vertebroplasty is a percutaneous procedure with a low complication rate that provides immediate and long-term pain relief to patients suffering from chronic vertebral compression fracture pain. Vertebroplasty is a minimally invasive procedure that not only provides immediate relief but continued and prolonged relief that may increase the patient’s daily activity level, which in turn helps provide a better quality of life. In several studies it has been shown that in more than 90% cases it provide immediate pain relief.
